Medi-Cal Rx Starting January 1, 2022
On January 1, 2022, the Department of Health Care Services (DHCS) will change the pharmacy benefit for Medi-Cal members. Their prescription medications will be covered by a new program called Medi-Cal Rx. This does not change their Medi-Cal eligibility or benefits. This does change the formulary for Medi-Cal members.
This does not affect members of Healthy Workers HMO.
If the member is eligible for both Medicare Part A, Part B, and/or Part D as well as Medi-Cal, Medicare will continue to be the primary insurance coverage wherever it is applicable.
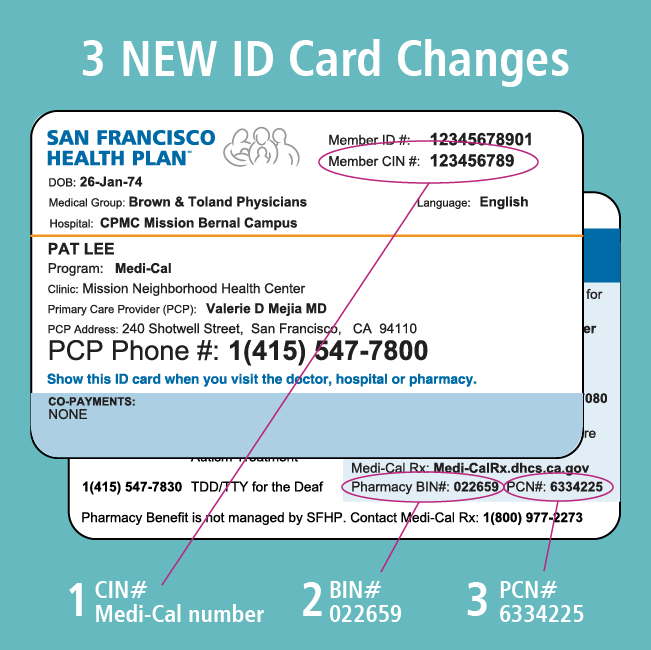
Prescription Billing for Medi-Cal Members After Medi-Cal Rx Transition (1/1/2022 and after): SFHP will issue new identification cards to all members to include the Medi-Cal CIN number, which must be used for Medi-Cal Rx billing.
| BIN | PCN | Group |
|---|---|---|
| 022659 | 6334225 | Medi-CalRx |
| Medi-Cal Rx Customer Service Center 1(800)-977-2273 https://www.medi-calrx.dhcs.ca.gov | ||
Starting January 1, 2022, prescriptions that are filled at a pharmacy will be covered by Medi-Cal Rx instead of SFHP. Medi-Cal Rx is a new program provided by the DHCS to provide pharmacy benefits for Medi-Cal members. DHCS is working with a new vendor called Prime Therapeutics to provide Medi-Cal Rx services.
There is no change to the physician-administered drug (PAD) benefit and PADs will continue to be covered by SFHP when billed as a medical claim with HCPCS code (and including NDC when required).
The Healthy Workers HMO pharmacy benefit is not changing.
Pursuant to Governor Newsom’s January 7, 2019 Executive Order N-01-2019, Medi-Cal pharmacy benefits will be transitioned to and thereafter administered through the fee-for-service delivery system for all Medi-Cal beneficiaries (generally referred to as “Medi-Cal Rx”). Transitioning pharmacy services from Medi-Cal managed care to fee-for-service will, among other things:
- Standardize the Medi-Cal pharmacy benefit statewide, under one delivery system.
- Improve access to pharmacy services with a pharmacy network that includes the vast majority of the state’s pharmacies and is generally more expansive than individual Medi-Cal managed care plan pharmacy networks.
- Apply statewide utilization management protocols to all outpatient drugs, as appropriate.
- Strengthen California’s ability to negotiate state supplemental drug rebates with drug manufacturers as the largest Medicaid program in the country with over 13 million beneficiaries.
Most SFHP members will be able to use the same pharmacy they do now on January 1, 2022. If their pharmacy is not contracted with Medi-Cal Rx, the member may need to choose another pharmacy. The pharmacy locator is available at https://www.medi-calrx.dhcs.ca.gov. Medi-Cal Rx does not have a preferred specialty pharmacy. Medi-Cal Rx does maintain contractual relationships with various specialty pharmacy providers, including SFHP’s specialty pharmacy, US Bioservices.
Medi-Cal Rx Secure Provider Web Portal medi-calrx.dhcs.ca.gov has key functions for provider and prescribers such as:
- Prior Authorization Information and Submittal Instructions
- Beneficiary Eligibility Look Up
- Web Claims Submission, Activities, and Inquiries.
Registration requires a PIN that providers will need to have sent to their enrolled practice address. For this reason, full registration takes at least a week and potentially longer.
For detailed registration and training instructions, access the Medi-Cal Rx Web Portal and Training Registration article located on the Pharmacy News Page or visit medi-calrx.dhcs.ca.gov/provider/ and click Register in the upper right hand corner.
Yes, Medi-Cal Rx has their own formulary called Contract Drug List (CDL). It is available on the Medi-cal Rx DHCS website.
- If the member was on a medication prior to 1/1/2022 through SFHP, the same medication will be “grandfathered” for a 180-day transition period. This means the members can continue to receive the same medications without prior authorization through June 2022. During the 180-day transition period, the provider will need to submit a prior authorization for members to continue on the medication, or switch to an alternative that is on the CDL.
- If the member has never received the medication using their Medi-Cal benefit prior to 1/1/2022, the provider will need to obtain a prior authorization from Medi-Cal Rx.
For drugs billed as pharmacy claims (prescriptions that members pick up from a pharmacy), providers can submit prior authorization (PA) requests through Medi-Cal Rx Provider Portal, fax, or mail. To submit a request:
- Fax requests for prior authorizations and attachments to 1-800-869-4325
- Enter PA information on Medi-Cal Rx provider portal https://www.Medi-CalRx.dhcs.ca.gov (registration required—see Portal information above)
- Submit PA electronically through CoverMyMeds®
- Mail PA requests to Medi-Cal Rx Customer Service Center, Attn: PA Request, PO Box 730, Sacramento CA 95741-0730.
Providers can check on the status of requests on Medi-Cal Rx Provider Portal or by phone to Medi-Cal Rx Call Center Line 1-800-977-2273. Please refer to https://www.Medi-CalRx.dhcs.ca.gov.
For physician-administered drugs (PADs) billed as medical claims (drugs billed to SFHP or one of our delegates as a HCPCS code), providers can continue to submit requests through the SFHP Portal, ProviderLink, or by fax at 1(415) 357-1292. There is no change to the PAD benefit and PAD will continue to be reviewed and covered by SFHP and its delegates.
Authorizations will be carried over or “grandfathered” for their originally approved dates of service up to 1 year, unless the drug is included in the list of exceptions for certain drug classes/categories (list below). New prior authorizations will be required from Prime Therapeutics after the original prior authorization expires.
Drug classes/classifications allowing for extended/multi-year PAs up to 5 years include:
Diabetes (insulin and anti-diabetic drugs), Asthma/COPD (long and short acting bronchodilators, inhaled corticosteroids and combination products, antihistamines, epinephrine), Antidepressants, Anticonvulsants, Anti-Parkinson’s, Immunosuppressants (for prevention of transplant rejection and treatment of autoimmune disorders), Cardiovascular drugs (including antihypertensives, antiarrhythmics, alpha and beta blockers, inotropics, diuretics), Agents for chronic treatment of Rheumatoid Arthritis, Pulmonary Hypertension, Multiple Sclerosis, Attention Deficit Hyperactivity Disorder (ADHD), Alzheimer’s Disease, Gout, Antihyperlipidemics, Contraceptives, Glaucoma Agents, Hormone replacement, Thyroid disorders, drugs for overactive bladder, nasal steroids, treatment for allergies and cough.
Starting on January 1, 2022, providers can call the Medi-Cal Rx Call Center Line at 1(800) 977-2273 (TTY: Dial 7-1-1) and a representative from the Medi-Cal Rx team at Prime Therapeutics will be able to assist 7 days a week, 24 hours a day.
If providers have questions before January 1, 2022, please contact the SFHP Provider Relations Department.
Phone: 1(415) 547-7818 ext 7084
Email: provider.relations@sfhp.org
Prior to 1/1/2022, providers can contact SFHP Pharmacy Department at 1(415) 547-7818 x7085.
On 1/1/2022 and after, please contact Medi-Cal Rx Call Center Line at 1(800) 977-2273.
Additional information
For more information about Medi-Cal Rx, click on the links below: